Scleral 2.0 Lens
The Scleral 2.0 Lens is the next evolution in custom-fitted scleral lenses.
Like the PROSE lens, each Scleral 2.0 Lens is custom made to perfectly fit your eye, allowing us to deliver lenses that help our patients see as clearly and comfortably as possible—but at a fraction of the cost and time commitment needed for a PROSE lens.
This system uses light waves to obtain over 1 million measurements of your eye with a precision of .01 millimeters. Complex algorithms combine these data points to create a precise topographical map of your cornea and sclera (the white parts of your eye). This data is used to deliver a uniquely shaped lens that perfectly fits your eye.
Because these lenses fit so well, we are able to incorporate the exact amount of prescription needed to provide the best vision possible. Even if you have extremely high astigmatism, you’ll be able to enjoy consistent, non-fluctuating, best-in-class vision.
We also can design lenses that go over lumps and bumps on your eyes, such as pingueculas and pterygiums. From the earliest stages of keratoconus to transplanted corneas, these lenses provide the best vision and comfort available.
Our doctors have seen countless patients throughout the years. Here are some of the frequently asked questions about scleral lenses.
Once you receive your lenses, we have scleral lens instructions on how to use and care for them.
How do I know if my eye doctor has the ability to create a custom scleral lens that perfectly matches my eye?
Ask your doctor if they offer corneal-scleral topography. Not just a corneal topographer but a specialized topographer that maps out the shape of the white part of your eye to make a completely custom scleral lens.
Standard Glasses
Many patients see clearly with normal glasses during the early stages of keratoconus. The exact powers you need are determined through a vision test called a refraction.
During a refraction, we ask you to repeatedly compare your vision through two different lenses: “Which lens is better, one or two?”
Here are some tips to ace this test:
- It’s important to know that you have three choices: “One is better,” “Two is better,” or “I can’t tell which lens is better.” All three options are valid and help us doctors figure out your exact power.
- Do not say that a particular lens is better if you can’t tell the difference. This may lead us to an incorrect glasses prescription.
- Sometimes, both options are not clear. You may be tempted to squint—but don’t! Instead, pick the option that is the better of the two options.
- It’s okay to ask to see the lens options again to help you compare differences and make the correct decision. However, remember that your first impression is often the right one.
- Keep trying your best even if you feel like you’re not doing well. The more advanced your keratoconus is, the harder it is to know which lens is better. Each answer you give helps us get closer to your perfect prescription.
Remember that you are not alone during this test.
We are here to guide you. Also, we use data from multiple sources to determine your glasses prescription—not just your answers. So don’t worry if you feel like you’re having a hard time. We’ve got a lot of experience working with tricky keratoconus prescriptions.
That being said, the value of an experienced doctor performing the refraction cannot be overstated, especially if you have keratoconus. Be cautious if a nurse or technician performs this measurement, since a complete understanding of the intricacies of the visual system is needed to precisely determine the prescription that will work for you.
Finally, as keratoconus progresses, the shape of your corneas will change.
These changes often result in large amounts of astigmatism and higher glasses prescriptions.
If you have a strong glasses prescription, make sure to utilize high-index lens materials. This material gives you thinner lenses and a more flattering lens shape. Also, purchase the best anti-glare coating you can afford. Anti-glare coatings make your vision better by reducing glare, light scatter, and reflections that reduce optical clarity. These options may increase the cost of your glasses, but most people find the investment in quality lenses to be well worth the cost.

Standard, Extended Range, and Custom Soft Contact Lenses
Soft contact lenses are available in a wide variety of sizes, materials, and powers. During the first stages of keratoconus, you’ll find that you can see clearly with standard soft contact lenses.
Unfortunately, as your keratoconus advances, your prescription will become higher and more abnormal. Eventually, the exact power necessary to provide clear vision may not be available in standard contact lens powers. At this point, you may benefit from extended range contacts, which are produced in a wider range of powers.
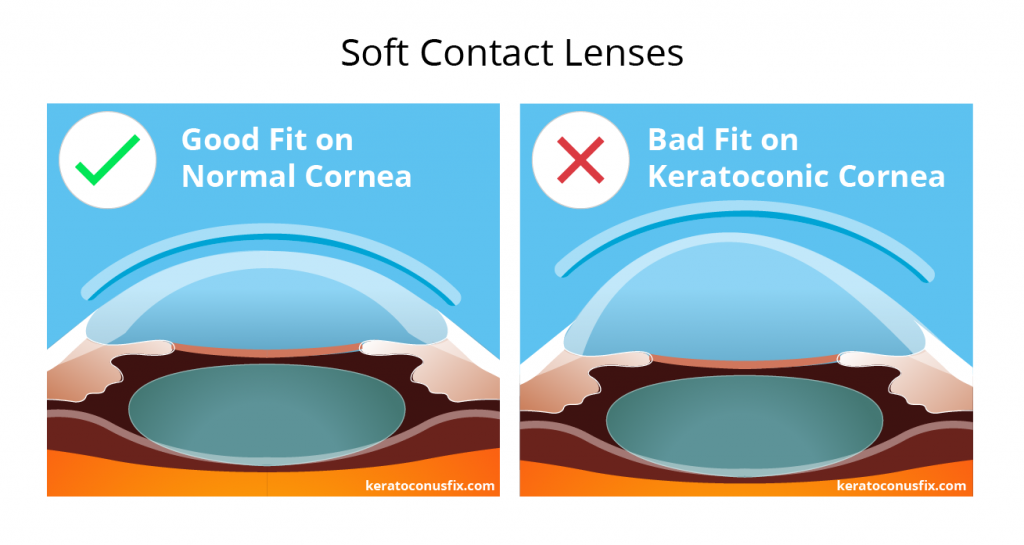
Alternatively, if extended range contacts don’t work well, custom-made soft contact lenses can be created for you. These contacts may have one month, three month, or even longer disposal schedules, allowing you to use the same lens for longer periods of time before needing to throw them away.
For many people, contacts are a good solution, but they’re not perfect.
Remember that clear and stable vision becomes harder to obtain as your prescription grows and your corneas become more irregular. Also, your eyelids may push on your lenses during blinks, causing the contact lenses to slightly move. These tiny movements can make a big difference, and many patients notice mild vision fluctuations with every blink.
The increased complexity of these lenses may require a greater number of contact lens follow-up appointments. Also, due to the custom-made nature of these contacts, these lenses may require more time to be delivered to your eye clinic. Through special arrangements, we are usually able to get them within a week or two, but clinics without special arrangements may have to wait up to two months, so please be patient with your local eye clinic.
Tip: If you are working with a clinic that experiences longer wait times, return for a yearly contact lens refit at least a month before you run out of your personal lens supply to ensure you always have a ready supply of contact lenses to wear.
Rigid Gas Permeable (RGP) Contact Lenses
Imagine a car with a windshield that has melted and warped due to excessive exposure to heat. It is impossible to clearly see through this misshapen windshield because of the distortion created by the irregular glass. Even if you put the best pair of lenses in the world in front of this windshield, you will not see clearly because the windshield is the problem—and no pair of glasses can fix that.
Similarly, as keratoconus advances, your corneas may become distorted. At this point, even the best pair of glasses or contacts will not provide clear vision. This is the time when rigid gas permeable lenses may be a good option for you.
Rigid gas permeable lenses are not soft like standard contact lenses.
In fact, they are often called “hard” contacts. They are inflexible and will break if you pinch them between your fingers with sufficient force.
Each lens is custom made, and many parameters must be specified by your doctor to provide good vision and comfort. Not all eye doctors are proficient fitting these lenses, so be sure to ask your eye clinic if they offer this service before making an appointment.
In the beginning, the rigid shape of these lenses make them very uncomfortable. Imagine putting tiny plastic plates on your eyeballs! Your first experience with RGP lenses will likely be a tearful event as your eye attempts to wash out the offending RGP lenses.
Eventually, however, your lenses may feel very comfortable as your eye adapts. Patients who have worn RGP lenses for many years often report them to be very comfortable. Unfortunately, if your eye has advanced keratoconus or if the shape of your eye is constantly changing, this level of comfort is difficult to achieve—and may not even be possible.
The reason why many people with keratoconus wear RGP lenses is because they provide clearer vision than glasses or soft contacts. The rigid lens acts as a replacement surface for your cornea. Corneal deformities are masked by the smooth regular surface of the lens, resulting in clearer vision.
Unfortunately, a poorly fitted RGP lens can damage the cornea.
If any part of your cornea rubs on the lens, scars may form, permanently reducing your ability to see. Therefore, it is important to have your eyes examined regularly by your eye doctor to ensure that the lens fits well and your changing eye does not put you at risk for corneal scarring.
Another drawback of this lens is reduced comfort.
If a speck of dirt becomes lodged between the lens and your eye, you’ll feel very sharp, intense eye pain and your eyes will water a lot. Also, these lenses may occasionally move off your cornea to the white part of your eyes, the sclera. This causes a strong feeling of discomfort, similar to having eyelashes stuck in your eye. On rare occasions, they may even pop out of your eyes. These contact lenses are almost impossible to find if they fall on the ground.
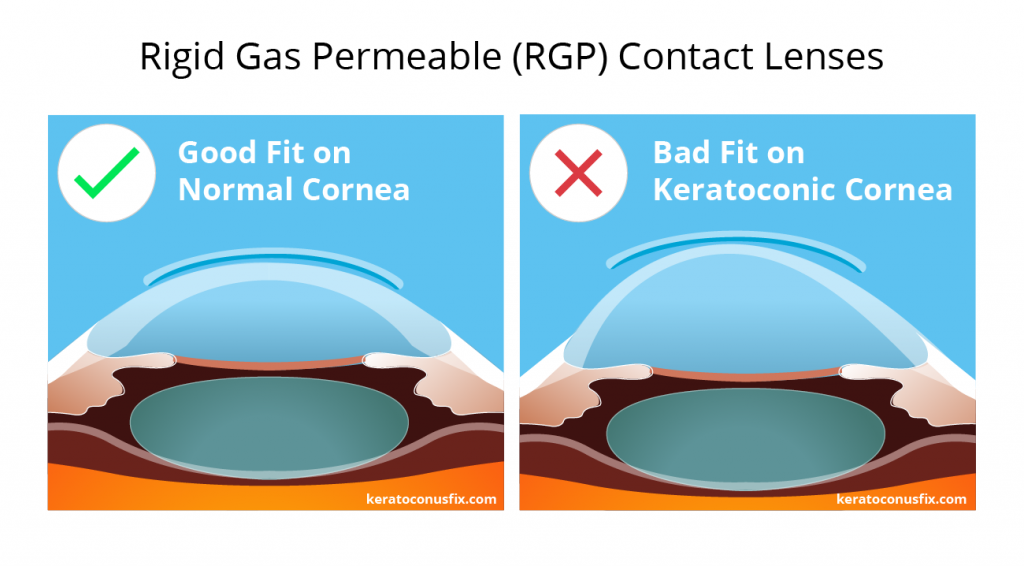
Finally, if your corneas become extremely distorted, it may become impossible to design a well-fitting RGP lens. Similar to balancing a plate on top of a pyramid, even the best doctor is unable to balance an RGP lens on an extremely irregular cornea. At that point, other options must be considered.
'Piggybacking' Contact Lenses
As your keratoconus progresses, it will become harder and harder to design a lens that is stable on your cornea. Eventually, your rigid gas permeable lens (RGP) will move so much that your vision will become intolerably unstable and uncomfortable. Also, your lens may rub against your eye in a way that damages your cornea. At this point, we may consider using both hard contact lenses and soft contact lenses on your eyes at the same time. This technique is called “piggybacking.”
With piggybacking, a larger, soft contact lens is first placed on the eye. Then, a smaller, hard contact lens is placed on top of the soft contact lens.
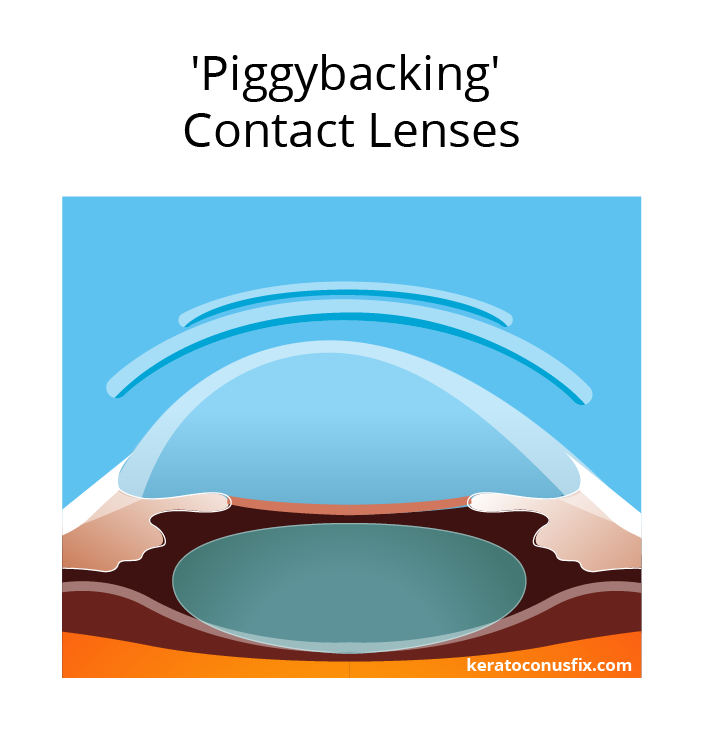
This technique allows you to enjoy the best of both worlds by using hard and soft contact lenses at the same time. The hard contact lens masks distortions in your cornea. This improves your vision. The soft contact lens acts as a cushion, protecting your eye from the hard contact lens and preventing the hard edges of RGP lenses from rubbing on your cornea. This results in improved comfort.
Unfortunately, maintaining a set of soft contacts and hard contact lenses is a lot of work.
You may find it to be inconvenient to insert and remove four different lenses every day. It’s also time-consuming and costly to clean and disinfect four lenses every night. Like many people, you may find this system requires too much effort to be worth it, especially compared to other treatment options.
Therefore, piggybacking is often recommended as a short term treatment option or if no other treatment option is available.
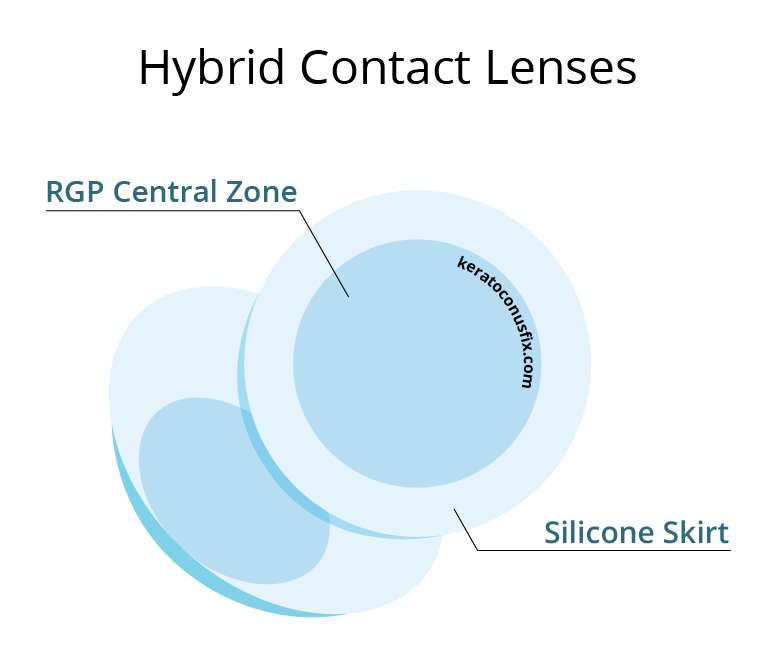
Hybrid Contact Lenses
Hybrid contacts combine the benefits of hard and soft contact lenses into a more convenient package. These lenses have a hard rigid gas permeable (RGP) center surrounded by a skirt of soft contact lens material.
Like RGP lenses, your vision may be better in hybrid contact lenses compared to glasses or soft contacts. The centers of hybrid lenses work exactly like hard lenses, replacing the distorted optics of your cornea with a smooth curved lens.
Unlike RGP lenses, however, these tend to be more comfortable when you first try them on because the soft skirt prevents the sharp RGP edges from rubbing against your eyes and eyelids in an uncomfortable way. Also, because of their larger size, these lenses are often more stable, moving less when you blink.
These lenses were initially designed for normal eyes. Therefore, first generation hybrid lenses are not a good option for eyes with keratoconus. However, the latest generation of hybrid contact lenses are able to be worn with irregular corneas, and this may be an option for you.
Hybrid lenses for keratoconus require special care when inserting them into your eyes.
The bowl of the lens must be filled with preservative-free saline and the lens must be placed on your eye to trap the saline between the lens and your eye. This technique allows the peaks of your irregular corneas to safely remain under the lens without rubbing against it, which may cause scarring. When putting on your lenses in the morning, avoid pushing the lens with too much pressure because this may cause the lens to rub against your cornea and damage your eye.
The drawback of hybrid contact lenses is our inability to completely customize the lens.
This limits our ability to provide the clearest vision possible, especially if you have astigmatism. Because these lenses are challenging for doctors to fit, many patients end up with contacts that are too tight or poorly fitting. This brings unwanted complications that often forces patients out of these lenses.
Finally, if your keratoconus is very advanced, it may be extremely difficult or impossible to design a lens that properly fits your eye and provides clear vision. Therefore, most specialty contact lens eye doctors have moved away from this technology for eyes with moderate or advanced keratoconus.
Standard Scleral Lenses
Scleral lenses are a good option for the vast majority of people with keratoconus. These lenses provide the clearest vision possible by replacing the poor optics of your distorted cornea with a perfectly smooth lens. Because of their large size and the way they fit, they are much more stable than hard rigid gas permeable (RGP) contacts. That’s why scleral lenses are the preferred choice for clear, consistent, non-fluctuating vision for people with keratoconus.
The cornea is the clear dome of tissue that sits in front of the colored parts of your eyes. The beauty of scleral lenses and the reason they work so well is because they are large enough to completely cover your corneas without actually touching them. In fact, they only touch the white part of your eyes.
Think about how sensitive your corneas are. Even the slightest touch makes your eyes water. Even worse, if you touch your corneas, you can damage them and develop permanent cloudy scars, which make clear vision impossible. That’s why doctors agree that it’s best to minimize rubbing between your cornea and contacts.
Fortunately, the white tissues of your eyes are actually very tough. Scleral lenses take advantage of this and rest completely on the white tissues of your eye. In fact, a properly fitted scleral lens should never touch your cornea at all!
This design makes scleral lenses extremely comfortable. Most patients are surprised at how comfortable they are when they first try them on. Most importantly, however, a properly fitted scleral lens eliminates the possibility of corneal scarring caused by the cornea and lens rubbing together.
Finally, scleral lenses are completely customizable. This allows us to design lenses that fit a wide variety of eyes. From the beginning stages of keratoconus all the way to the most advanced stages and even on to transplanted corneas—scleral lenses are a safe and healthy way to give you the best vision possible.
First Generation Lenses
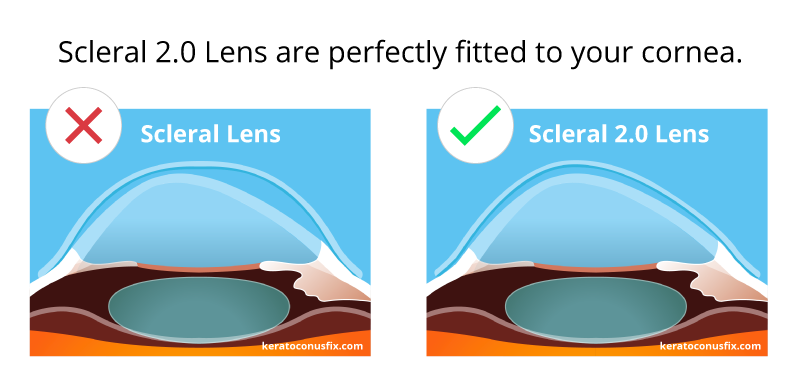
In the early days of scleral lenses, we thought that most eyeballs were round. Looking back, we now realize that this assumption was completely wrong! The vast majority of eyeballs are not round. In fact, a recent study found that only 5% of eyeballs are round.
Due to limited technology, the first scleral lenses were only capable of being designed to fit on round eyeballs. Back then, we didn’t have the ability to completely customize our lenses, either. So, during the fitting process, we picked a small, medium, or large lens and tinkered with different curvature rates until we got the best fit we could. As you can imagine, getting a perfect fit was challenging.
Think about it. Imagine you had a lens that was shaped like half a basketball. Now try fitting that perfectly round lens on a football. The football just wobbles inside the round lens. It doesn’t fit the football at all. It just doesn’t work.
In the same way, using a perfectly round scleral lens on a football shaped eye doesn’t work. If you try this, you’ll find that some areas are too tight, causing pinching and painful pressure on your eyes. You’ll also find that other areas are too loose, making you to feel the edge of the lens every time you blink.
This is why first generation scleral lenses were often uncomfortable. Also, these poorly fitting lenses often caused problems such as mid-day fogging and painful red eyes.
Second Generation Lenses
After we realized that that most eyeballs are football shaped, we started designing lenses to fit on footballs. This worked better and patients were happier. However, we still had a problem: We could change the lens to fit footballs and they were longer, shorter, thinner, and wider—but we always had to assume the eye was shaped like a perfectly symmetric football.
Now we know that eyeballs are not shaped like perfect footballs. In fact, recent studies have revealed that only 30% eyeballs are shaped like footballs. 65% of eyes are not perfectly symmetrical and do not have uniform curves like a football. Unfortunately, the majority of doctors who fit scleral lenses are unable to take advantage of this research because they don’t have the technology to create a custom scleral lens that perfectly fits a patient’s unique eye.
This is why fitting a scleral lens isn’t easy for most doctors. Some doctors struggle with lens after lens, trying to find a good fit through trial and error. We’ve heard stories of patients seeing their doctor more than ten times to try on ten different lenses and still being unable to get a lens that works. It’s frustrating, time consuming, and costly for both patient and doctors alike.
Prosthetic Contact Lenses
BostonSight recognized this problem and developed a system in 1994 that captures a mold of your eye and creates a lens that fits the unique shape of your eye. They call it a Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) lens.
These lenses are only available in twelve universities in the United States. They cost an average of $15,000 for one set of lenses. The fitting process is rigorous, taking four to twelve day long visits to complete the treatment, with follow up visits as needed during the first six months of wear.
If you are near one of these eye clinics, are able to make an appointment, and don’t mind the time commitment and financial costs, then go for it.
But if not, then read on…
Our process
We promote a customized Scleral 2.0 Lens experience.
- 1
Scleral 2.0 clinics
We have convenient locations in Southern California and the greater Seattle area. Each location is equipped with Scleral 2.0 Lens technology.
Find a clinic - 2
Free Initial Consultation
We'll set up a complimentary initial 10-minute phone consultation with a doctor. We'll discuss your particular visual needs and determine whether you are a good candidate for this procedure.
Schedule a call - 3
Initial Eye Exam
If you are a good candidate, you’ll be invited to our clinics for an eye exam, lens measurements, and vision evaluation with a lens demonstration. The demonstration lens will not be your final lens, but allows you to experience what it’s like to wear a scleral lens, and to experience the clarity you will be able to achieve.
Schedule an exam - 4
Lens Production
Once you feel comfortable and agree to move forward, fabrication of your lens will begin. After 14 days, your completely customized lens will be available for your first fitting and you’ll be called in.
- 5
First Fitting
During this examination, we will evaluate the fit, comfort, and vision of your custom scleral lenses. We will take measurements and assess your vision. We will also set aside time to teach you how to insert and remove the lens and how to properly maintain your lens.
Schedule a fitting - 6
Fine Tuning
If changes are needed, this data will be used to make a new lens, and you’ll be called in again. These fitting sessions will be repeated until you’re seeing as clearly as possible. At this point, you will take your lenses home for a few days to see how your eyes adjust to them.
- 7
Final Lenses
After you return and confirm that the lenses are working well, we will finalize the lenses. They are now yours to keep.
